Sugammadex Sodium is a novel antagonist of selective non-depolarizing muscle relaxants (myorelaxants), which was first reported in humans in 2005 and has since been used clinically in Europe, the United States and Japan. Compared with traditional anticholinesterase drugs, it can antagonize deep nerve block without affecting the level of hydrolyzed acetylcholine at cholinergic synapses, avoiding the adverse effects of M and N receptor excitation, and greatly improving the quality of post-anesthesia awakening. The following is a review of the recent clinical application of sodium sugars in the wake period of anesthesia.
1. Overview
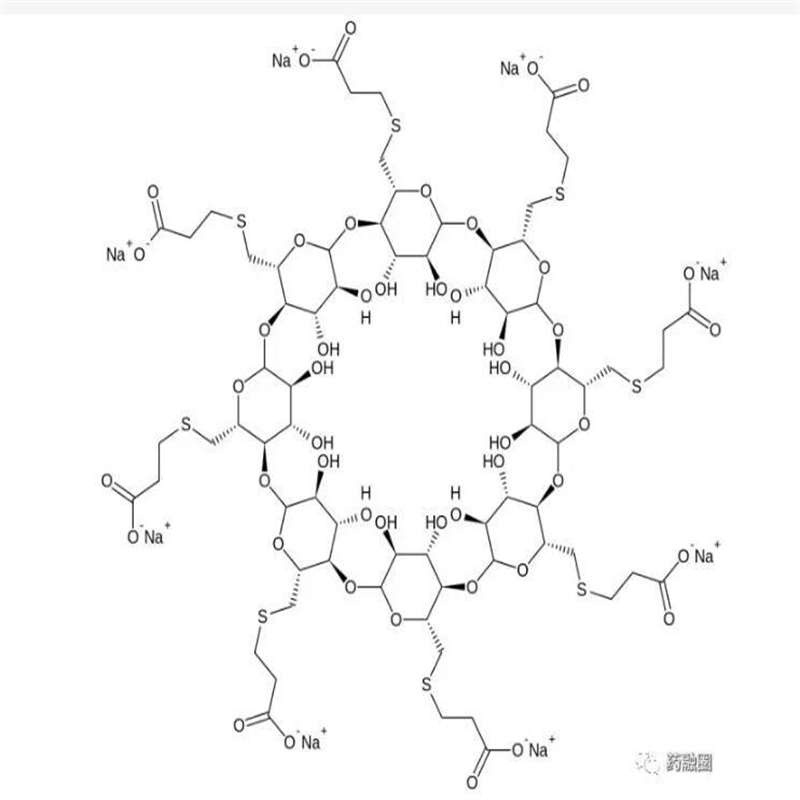
Sugammadex Sodium is a modified γ-cyclodextrin derivative that specifically reverses the neuromuscular blocking effect of steroidal neuromuscular blocking agents, especially rocuronium bromide. Sugammadex Sodium chelates free neuromuscular blockers after injection and inactivates the neuromuscular blockers by forming a stable water-soluble compound through a 1:1 tight binding. By such binding, a concentration gradient is formed that facilitates the return of the neuromuscular blocker from the neuromuscular junction to the plasma, thereby reversing the neuromuscular blocking effect it produces, releasing nicotinic acetylcholine-like receptors and restoring neuromuscular excitatory transmission.
Among the steroidal neuromuscular blockers, Sugammadex Sodium has the strongest affinity for pecuronium bromide, followed by rocuronium, then vecuronium and pancuronium. It is worth noting that to ensure faster and more effective reversal of neuromuscular blocking effects, an excessive amount of Sugammadex Sodium should be used relative to the myorelaxants in circulation. In addition, Sugammadex Sodium is a specific antagonist of steroidal neuromuscular blocking agents, and it is unable to bind benzylisoquinoline non-depolarizing myorelaxants as well as depolarizing myorelaxants, and therefore, cannot reverse the neuromuscular blocking effects of these drugs.
2. Efficacy of sugammadex sodium
In general, the dose of muscarinic antagonists during anesthetic awakening depends on the degree of neuromuscular blockade. Therefore, the use of a myoson monitor facilitates the rational application of neuromuscular blocking antagonists. The myorelaxation monitor dispenses electrical stimulation delivered to peripheral nerves, causing a motor response (twitching) in the corresponding muscle. Muscle strength decreases or disappears after the use of myorelaxants. As a result, the degree of neuromuscular blockade can be graded as: very deep block [no twitching after either four train-of-four (TOF) or tonic stimulation], deep block (no twitching after TOF and at least one twitching after tonic stimulation), and moderate block (at least one twitching after TOF).
Based on the above definitions, the recommended dose of sodium sugars to reverse moderate block is 2 mg/kg, and the TOF ratio can reach 0.9 after about 2 min; the recommended dose to reverse deep block is 4 mg/kg, and the TOF ratio can reach 0.9 after 1.6-3.3 min. For rapid induction of anesthesia, high-dose rocuronium bromide (1.2 mg/kg) is not recommended for routine reversal of very deep block. However, in the case of an emergency return to natural ventilation, reversal with 16 mg/kg of Sugammadex Sodium is recommended.
3. Application of Sugammadex Sodium in special patients
3.1. In pediatric patients
Data from phase II clinical studies suggest that Sugammadex Sodium is as effective and safe in the pediatric population (including neonates, infants, children and adolescents) as it is in the adult population. A meta-analysis based on 10 studies (575 cases) and a recently published retrospective cohort study (968 cases) also confirmed that the time (median) for recovery of the ratio of the 4th myoclonic twitch to the 1st myoclonic twitch to 0.9 in subjects given rocuronium bromide 0.6 mg/kg and Sugammadex Sodium 2 mg/kg at T2 presentation was only 0.6 min in infants (0.6 min) compared to children (1.2 min) and adults (1.2 min). 1.2 min and half of that of adults (1.2 min). In addition, one study found that Sugammadex Sodium reduced the incidence of bradycardia compared with neostigmine combined with atropine. The difference in the incidence of other adverse events such as bronchospasm or postoperative nausea and vomiting was not statistically significant. It has also been shown that the use of Sugammadex Sodium reduces the incidence of postoperative agitation in pediatric patients, which can be helpful in the management of the recovery period. In addition, Tadokoro et al. demonstrated in a case-control study that there was no correlation between perioperative allergic reactions to pediatric general anesthesia and the use of sodium sugammadex. Therefore, the application of Sugammadex Sodium is safe in pediatric patients during the awakening period of anesthesia.
3.2. Application in elderly patients
In general, older patients are more susceptible to the effects of residual neuromuscular blockade than younger patients, and spontaneous recovery from neuromuscular blockade is slower. In a multicenter phase III clinical study of the safety, efficacy, and pharmacokinetics of Sugammadex Sodium in elderly patients, they found that Sugammadex Sodium reversed rocuronium to produce a slight increase in the duration of neuromuscular blockade compared with patients younger than 65 years (mean times of 2.9 min and 2.3 min, respectively). However, several studies have reported that sugammadex is well tolerated by elderly patients and that no re-arrow toxification occurs. Therefore, it is considered that Sugammadex Sodium can be safely used in elderly patients during the awakening phase of anesthesia.
3.3. Use in pregnant women
There is little clinical guidance on the use of Sugammadex Sodium in pregnant, fertile and lactating women. However, animal studies have found no effect on progesterone levels during pregnancy and no stillbirths or abortions in all rats, which would guide the clinical use of Sugammadex Sodium during pregnancy, especially in the first trimester. There have also been a number of cases of maternal use of sodium sugars under general anesthesia for cesarean sections, and no maternal or fetal complications have been reported. Although some studies have reported a relatively small transplacental transfer of sodium sugars, there is still a lack of reliable data. Notably, pregnant women with gestational hypertension are often treated with magnesium sulfate. Inhibition of acetylcholine release through magnesium ions interferes with neuromuscular junction information transduction, relaxes skeletal muscle, and relieves muscle spasm. Therefore, magnesium sulfate may enhance the neuromuscular blocking effect of myorelaxants.
3.4. Application in patients with renal insufficiency
Sugammadex Sodium and sucralose-rocuronium bromide complexes are excreted by the kidneys as prototypes, so that the metabolism of bound as well as unbound Sugammadex Sodium is prolonged in patients with renal insufficiency. However, clinical data suggest that Sugammadex Sodium can be safely used in patients with end-stage renal disease, and there are no reports of delayed neuromuscular blockade after Sugammadex Sodium in such patients, but these data are limited to 48h after Sugammadex Sodium administration. In addition, the sodium sugammadex-rocuronium bromide complex can be eliminated by hemodialysis with high-flux filtration membranes. It is important to note that the duration of rocuronium reversal with sodium sugammadex may be prolonged in patients with renal disease. Therefore the use of neuromuscular monitoring is essential.
4. Conclusion
Sugammadex Sodium rapidly reverses the neuromuscular blockade caused by moderate and profound aminosteroid myorelaxants, and it significantly reduces the incidence of residual neuromuscular blockade compared with conventional acetylcholinesterase inhibitors. Sodium sugammadex also significantly accelerates the time to extubation during the awakening period, shortens the number of days of hospitalization, accelerates the recovery of patients, reduces hospitalization costs, and saves medical resources. However, allergic reactions and cardiac arrhythmias have been reported occasionally during the use of Sugammadex Sodium, so it is still necessary to be vigilant during the use of Sugammadex Sodium and to observe the changes of patients'vital signs, skin conditions and ECG. It is recommended to monitor skeletal muscle contraction with a muscle relaxation monitor to objectively determine the depth of neuromuscular blockade and use a reasonable dose of sodium sugammadex to further improve the quality of the awakening period.